Atypical Presentation of Multidrug-Resistant Acinetobacter baumannii Pneumonia in a Post-Surgical ICU Patient: A Case Report
Zaina Rawashdeh(1) • Marah J Alshatarat(1) • Basil G Daradkeh(2) • Dina Awwad(3) • Sara H Sawalha(1)
Published in Cureus Journal: 10.7759/cureus.89059
PubMed Index: PMC12398324
Abstract
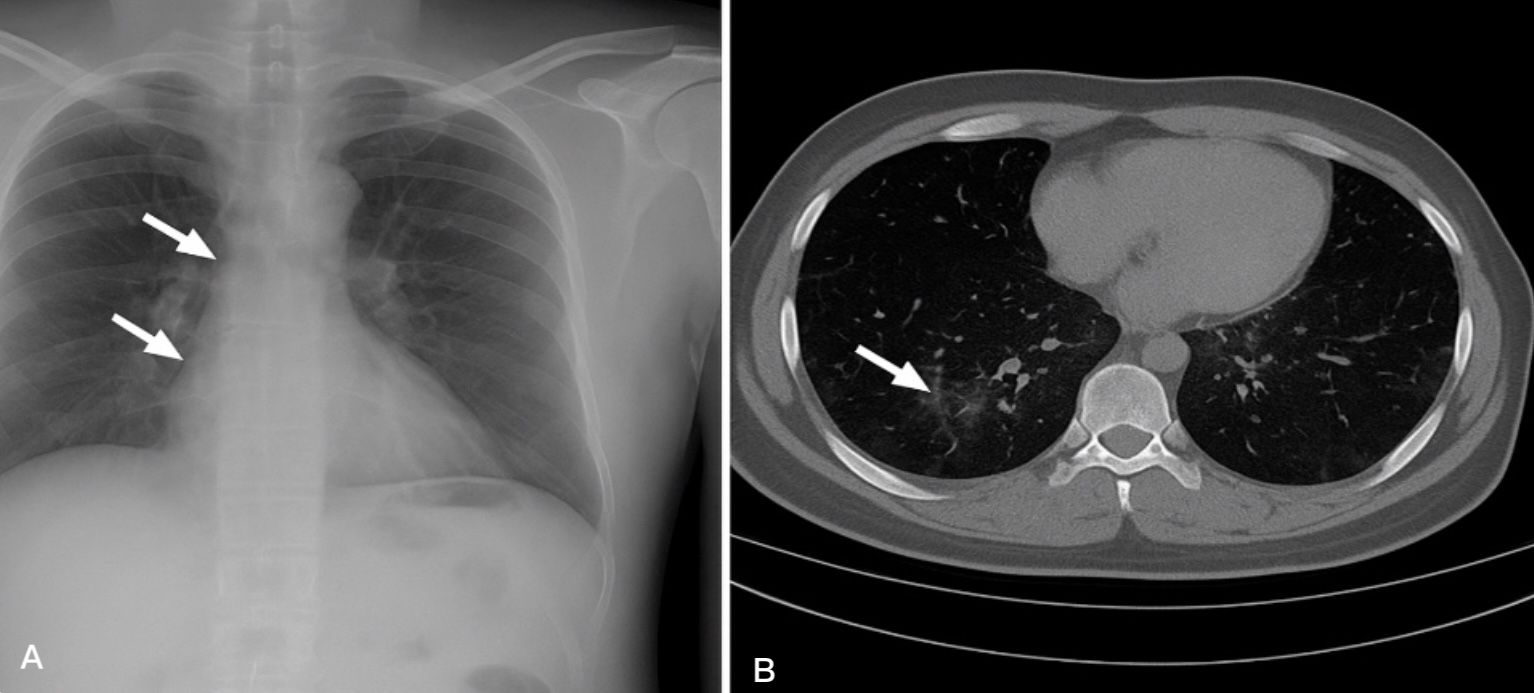
Acinetobacter baumannii is a Gram-negative opportunistic pathogen increasingly encountered in hospital environments, particularly in intensive care units (ICUs), where it presents a major clinical challenge due to its multidrug-resistant (MDR) profile. Its resistance to multiple antibiotic classes makes it a serious therapeutic challenge, particularly in post-surgical patients where symptoms may be atypical. We report a case of a previously healthy 64-year-old male patient with a history of hypertension and coronary artery disease, admitted to the ICU following elective abdominal aortic aneurysm repair. On postoperative day five, he developed mild respiratory symptoms, low-grade fever, and oxygen desaturation, but with no abnormal lung auscultation findings. Elevated inflammatory markers and radiologic evidence of faint bilateral perihilar infiltrates and subtle ground-glass opacities prompted further investigation. Cultures revealed MDR A. baumannii resistant to carbapenems, aminoglycosides, and fluoroquinolones, but susceptible to colistin and tigecycline. The patient received combination intravenous therapy with colistin and tigecycline, resulting in rapid clinical improvement, normalization of inflammatory markers, and complete radiologic resolution by day 14. This case underscores the importance of maintaining a high index of suspicion for MDR pneumonia in post-surgical ICU patients with non-specific symptoms and highlights the role of early diagnosis and targeted therapy in achieving favorable outcomes.
For Full Access click here