Perceptions of Fungal Contamination in Hospital Humidifiers Among Healthcare Providers in Jordan: A Cross-Sectional Study
Zaina Rawashdeh(1) • Mohammad A Al-Shalalfeh(1) • Abdulrahman M Alsarhan(1) • Leen O Sabbah(1) • Khaled Kettaneh(2) • Farah M Shahin(3) • Basil G Daradkeh(4) • Nour A Alaqgad(1) • Subhi M Nassar(1) • Nada M Abujbara(1)
Published in Cureus Journal: 10.7759/cureus.88721
PubMed Index: PMC12375258
Abstract
Background: Hospital-acquired infections remain a critical concern globally. Fungal contamination of reusable hospital humidifiers, especially in intensive care units (ICUs), represents an under-recognized threat. These devices, if improperly maintained, may become reservoirs for opportunistic pathogens such as Aspergillus and Fusarium, thereby compromising patient safety.
Objective: The objective of this study is to explore the perceptions of fungal contamination in hospital humidifiers across Jordan and describe associated disinfection practices, protocol presence, and staff awareness, with the aim of informing targeted preventive strategies.
Methods: A cross-sectional observational study was conducted from May 1 to June 1, 2025, using an anonymous, self-administered online questionnaire distributed via hospital email lists and official WhatsApp groups. Eligible participants included physicians, nurses, residents, medical students, and infection control staff from departments that regularly use humidifiers (e.g., ICUs, pediatrics, internal medicine, emergency medicine). The survey collected data on disinfection routines, protocol availability, and awareness of fungal risks. In total, 50 valid responses were analyzed. Descriptive statistics were used, and Chi-square and Fisher’s Exact Tests were applied to assess associations. However, the findings are limited by the reliance on self-reported data, the absence of microbiological validation, limited details on humidifier types and maintenance, potential departmental confounding, and the small convenience sample (n=50), which may affect generalizability. Ethical approval was not required under local guidelines, given the minimal-risk nature of the study.
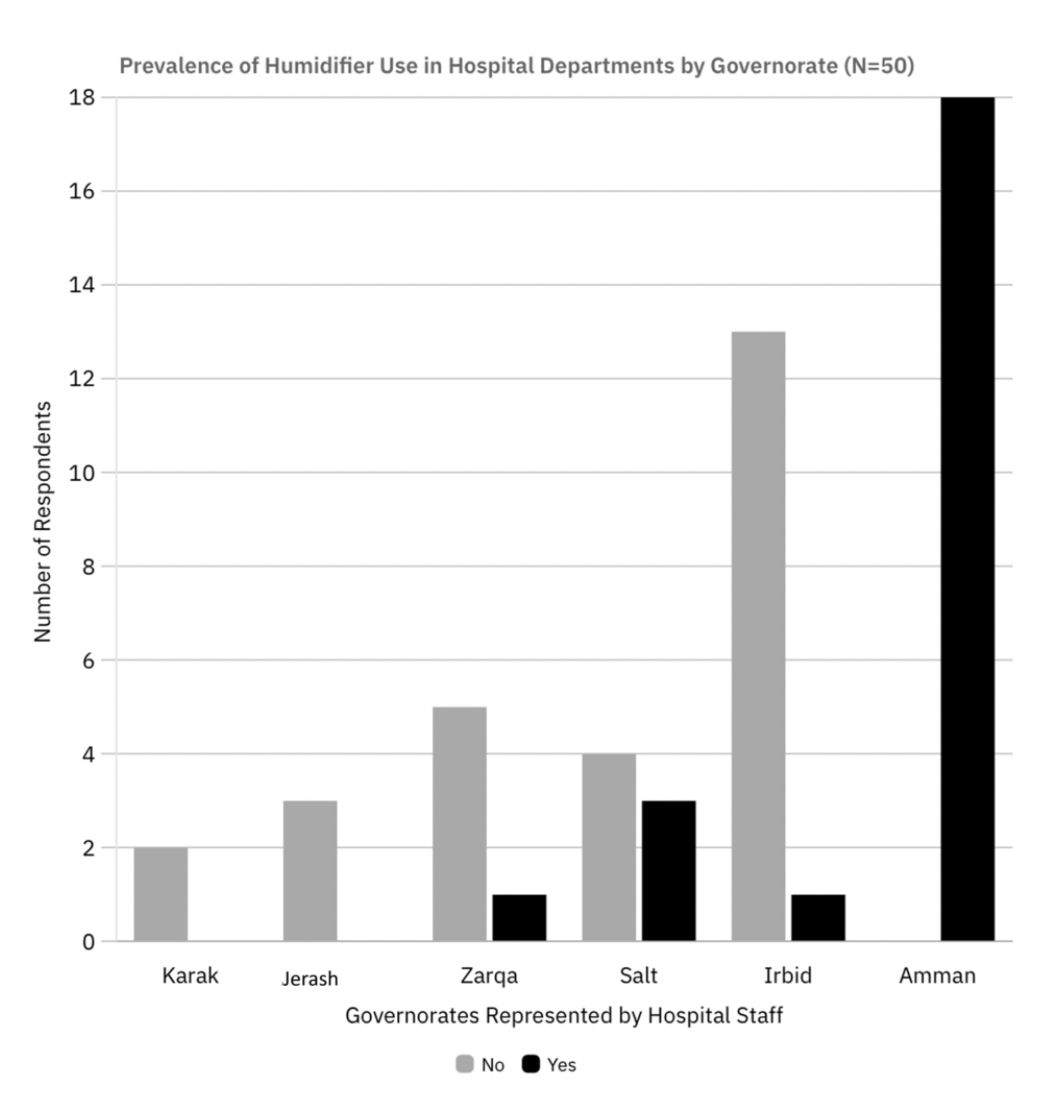
Results: Of the 50 valid responses, self-reported data showed that 29 participants (58%) observed previous fungal contamination in their department’s humidifiers. Contamination was reported in all humidifiers located in ICUs (n = 17, 100%) and general wards (n = 2, 100%). A statistically significant association was observed between cleaning frequency and contamination (p = 0.0034), with higher contamination among frequently cleaned devices. Geographic disparities were also noted, with Amman showing a 100% (n = 19) contamination rate, compared to 7.7% (n = 1) in Irbid (p < 0.001). While 44 (88%) participants were aware of fungal risks, only 27 (54%) reported having written cleaning protocols. Results are limited by reliance on unverified staff reports. Therefore, contamination rates were based on participant perception and may be influenced by department-specific practices or equipment use frequency.
Conclusion: Fungal contamination in hospital humidifiers is widespread, particularly in ICUs. The paradoxical association between frequent cleaning and higher contamination may reflect increased usage and confounding by department type. These findings highlight the urgent need for standardized protocols, microbiological monitoring, and staff training to mitigate nosocomial fungal infections in Jordan.
For Full Access click here